The Monaco Cardiothoracic Centre treats patients suffering from coronary artery disease and provides them all current medical, interventional cardiology, and surgical treatment options after discussion and decision by the medico-surgical staff depending on what is best suited to each patient at a given time.
What are the symptoms?
What causes it?
How is it diagnosed?
What treatments are available?
What is coronary artery disease?
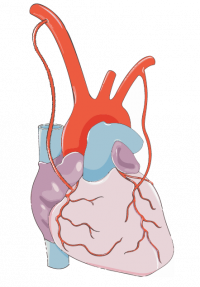
Coronary artery disease or coronaropathy are disorders affecting the arteries of the heart (coronary arteries) which narrow (stenosis) and reduce the flow of blood to the heart muscle (myocardium). Coronary artery disease is subject to risk factors for atherosclerosis.

SYMPTOMS
Symptoms of coronary heart failure vary from person to person, but the most common are :
- discomfort or pain in the chest (angina) such as clenching, burning
- pain in the shoulder or in the arm or in the jaw
- difficulty breathing – shortness of breath
- extreme fatigue during exertion
Women may experience atypical chest pain and digestive disorders. Pain can be fleeting or sharp and felt in the abdomen, back or arm. Nausea and back or jaw pain may also be a sign of heart attack in women.
CAUSES
Hardening of the arteries occurs with age. However, certain risk factors can accelerate the process :
- Age (over 45 for men and over 55 for women)
- Family history of heart disease
- Smoking
- High blood pressure
- A high level of “bad” LDL cholesterol and a low level of ” good ” HDL cholesterol
- Certain diseases, such as diabetes
- Being overweight or obese
- Lack of exercise
- Stress
DIAGNOSIS
The Monaco Cardiothoracic Centre has state-of-the-art infrastructures for comprehensive screening and diagnosis of the disease. The most common examinations are :
What is an exercise ECG?

It is used to measure the electrical activity of the heart, the blood pressure and the heart rate. The cardiologist can then analyse the impact of exercise on how your heart works and detect any disease.
Why should I take this test?
Depending on the person, a stress test can be taken for several reasons:
- To determine the cause of chest pain
- After a myocardial infarction (or “heart attack”), to monitor how the heart is working and to determine how much physical exercise it is safe to do
- To keep an eye on the progression of heart disease
- To monitor patients with cardiovascular risk factors, high-level athletes or sportspeople aged over 55.
How should I prepare for a stress test?
- Don’t fast. Eat normally, but not sooner than two or three hours before the test
- If you are taking any medication, continue to do so as usual (unless advised not to by your doctor)
- Don’t smoke for one hour before and one hour after the test
- Wear comfortable clothes and footwear, so you can walk or pedal quickly without discomfort. Put on a top that you can take off easily.
What happens during a stress test?
- It is usually performed in a clinic or hospital and consists of performing more and more intense physical exercises until fatigue sets in.
- It takes between 15 and 20 minutes.
- A stress test is conducted by a cardiologist assisted by a nurse, and takes place over three stages.
1. Consultation
The doctor will ask you about your family history and level of cardiovascular risk associated with smoking, whether you have diabetes, high cholesterol, hypertension or even obesity.
2. Physical examination
Before the test, a physical examination is performed: listening to the heart, lungs and taking blood pressure and heart rate.
3. The test
A stress test usually lasts about 15 minutes. It takes place in a cool room (18 to 20°C). It increases in gradual stages (every two or three minutes): the treadmill accelerates or the resistance of the bike increases every three minutes on average. The test stops if you become exhausted or significantly short of breath, if you reach the theoretical maximum heart rate, if your blood pressure becomes too high, if there is a problem with your heart rhythm or if you don’t feel well.
At the same time, the heart rate, the electrical activity of the heart and the blood pressure are recorded regularly, via the small electrodes attached to the chest.
All the time while you are exercising, you must tell the team about any abnormal symptoms (if you experience any discomfort, chest pain, tightness, shortness of breath, significant fatigue, abnormal heartbeat, etc.).
To ensure reliable results, the stress test usually continues until the heart beats as fast as possible (depending on the patient’s age and health). It is therefore important to keep making an effort until you feel tired.
4. After the test: recovery
When the stress test is over, you need to continue walking or pedalling more gently for a few minutes, to facilitate recovery. A period of complete rest may be needed.
At the same time, the cardiologist will carry on measuring your heart rate, its electrical activity and your blood pressure. This monitoring continues until normal values (measured at rest) are restored.
Contraindications
A stress test is not recommended if you have:
- recently had a heart attack
- unstable angina pectoris
- high blood pressure
- endocarditis
- myocarditis
- pericarditis
- respiratory failure
- arthritis
Faster and more efficient than previous scanners, the Naeotom Alpha scanner (Siemens Healthineers), with photon counting, allows a much finer definition and analysis of the coronary arteries, with less irradiation.
Why should I have a cardiac CT scan?
What happens during the exam?
What risks does it pose?

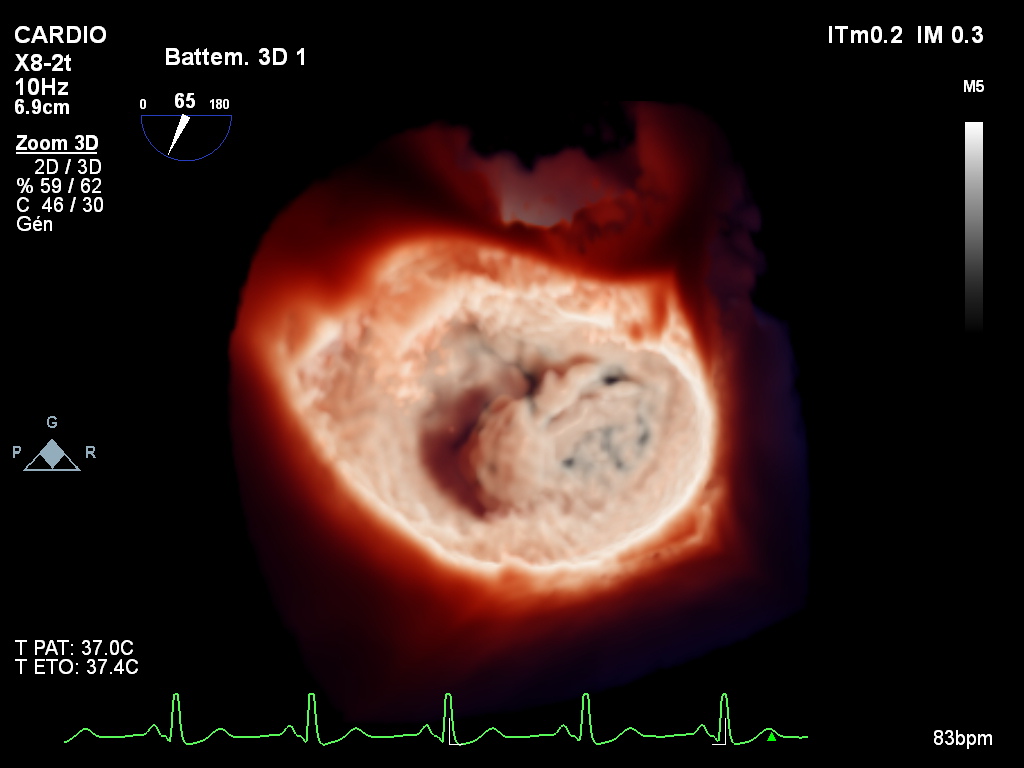
Studies the irrigation of the heart muscle by reproducing effort conditions (Adenosine) and it enables visualisation of the viable and non-viable areas of the heart muscle (Gadolinium).

This examination is performed by puncturing either the radial artery (at the wrist) or the femoral artery (in the groin fold).
It makes possible visualisation of the narrowing and occlusion of the arteries.
Combined with fractional flow reserve (FFR) measurement, it can assess whether coronary stenosis leads to a decrease in the blood supply of the heart muscle.
Other examinations can be performed, such as :
- Electrocardiogram (ECG)
- Myocardial perfusion scintigraphy
- Angiography
- Intravascular ultrasound
- X-rays
- Blood tests
Cardiac emergency: an optimal care pathway
The importance of coordination between professionals
Testimony of an active man, with no history of heart problems, who suddenly suffered a heart attack after his sports session and was treated at the CCM.
A life saved, a life that has changed. Monitor your heart health!
TREATMENT
In addition to medication and a strict lifestyle, surgical procedures can also be performed to improve blood supply to the heart.
Medical treatment and dietary rules
Performed under a local anaesthetic in a sterile hybrid interventional cardiology room, this procedure involves dilating the narrowed artery with a balloon and usually inserting a stent via the radial artery in the wrist or the femoral artery in the fold of the groin.
What is angioplasty?
Over time, fatty deposits can build up on the walls of the arteries. These plaques, known as atherosclerosis, consist of cholesterol, fibrous tissue and inflammatory cells. They gradually obstruct the vascular lumen and slow down the flow of blood.
If a coronary artery is affected by this phenomenon, it can disrupt blood flow towards the heart, which does not then receive enough oxygen. This can cause angina pectoris*, or in case of sudden total occlusion, a heart attack.
Coronary angioplasty is a technique to reopen narrowed or blocked arteries in the heart (coronary arteries), which restores blood flow towards the heart.
It is an invasive procedure performed by an interventional cardiologist, because it requires the insertion of a small probe (or catheter) into an artery either in the wrist (radial artery) or in the fold of the groin (femoral artery).
In most cases, a coronary stent is placed to make it easier for the artery to heal and prevent the rapid recurrence of narrowing.
It can either be scheduled or performed in an emergency in cases of acute coronary syndrome.
*Angina pectoris, or angina, refers to chest pain that usually appears during exertion, stress, or even at rest. ‘Angio-’ means “involving a blood vessel” and ‘-plasty’ means “repair”.
What is it for?
Angioplasty restores normal blood flow in the coronary artery to ensure optimal perfusion of the heart muscle, by dilating a coronary narrowing.
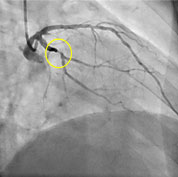
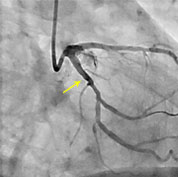
Narrowings of the coronary arteries, identified and accurately located by coronary angiography, can be treated by angioplasty with inflatable balloons and, most of the time, the placement of a stent.
Coronary angioplasty is indicated primarily in cases of acute coronary syndrome, i.e. unstable angina pectoris, to prevent a heart attack; during an acute heart attack (to unclog the occluded artery, preferably within three hours of the onset of symptoms); or in cases of failed thrombolysis (drug treatment to unblock the artery).
It is also indicated in stable coronary artery disease after discussion with a cardiologist and after individual evaluation of the expected benefits and risks to the patient.
What happens during the procedure?
Like the preceding coronary angiography, coronary angioplasty requires medical preparation. A blood test is requested to assess coagulation, complete blood count (looking for anaemia, signs of infection, abnormal platelet count, etc.) and kidney function.
The patient should be treated with antiplatelet drugs such as aspirin and other specific drugs for coronary artery disease, during or before the procedure.
It is performed in an interventional cardiology room, under local anaesthesia. It can be completed in outpatients or during a short, 24-hour admission.
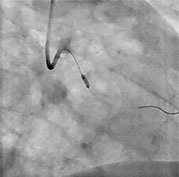
The interventional cardiologist inserts a hollow flexible tube (catheter), usually via the radial artery (in the wrist) or the femoral artery (in the groin). The technique then involves placing a small inflatable balloon into the narrowed area of the artery where there is a problem, carefully identified using contrast medium injected via the catheter.
Once in the correct position, the balloon is inflated for a few seconds to destroy the plaque of atherosclerosis and enlarge the diameter of the artery. The resolution of the narrowing is then checked using another injection of contrast medium into the artery being treated. It is then deflated to restart the circulation and restore blood flow.
Placement of a stent
In 90% of cases, an angioplasty is completed in this way. A stent is a kind of miniature spring, inserted into the artery to prevent it from becoming clogged again. The point of the procedure is to keep the artery open using the spring, which stays in place when the balloon is removed.
Cardiologists now have “active stents”, coated with drugs that inhibit cell proliferation in contact with the metal bars of the stent, which reduces the risk of restenosis, meaning further obstruction of the artery despite the stent.
What risks does angioplasty pose?
Thanks to improvements in equipment and medical teams, the risks associated with coronary angioplasty have been drastically reduced. However, this procedure remains an ‘invasive’ treatment.
A number of complications can occur during angioplasty or immediately afterwards.
Allergic complications: Usually related to the use of iodine-based contrast medium or local anaesthetic. If the patient has experienced allergic reactions in the past, you must tell the cardiologists and anaesthetists.
Complications at the puncture site: The most common complication is a small bruise, a patch of bluish skin that can persist for a few days but is usually inconsequential. Much more rarely, an artery can become clogged or injured and can require surgical repair and/or blood transfusion.
Cardiovascular complications: During angioplasty, there can be pain in the chest or palpitations caused by a heart rhythm disorder. Moving a clot, injury to an artery or other complications can require another angioplasty, coronary bypass surgery (emergency heart surgery), a heart attack or death. Fortunately, this kind of serious complication is very rare (fewer than 1 in 1000 cases).
After angioplasty
After angioplasty, most people are admitted to hospital to monitor their condition overnight. They can usually go home early the next day.
If a stent has been implanted, antiplatelet treatment – aspirin and clopidogrel – must be taken for at least the first few months, to prevent the blood from clotting over the metal stent. A lower, long-term dose of this treatment will then be prescribed by your cardiologist.
You can resume your usual activities, including sport, within a few days. Your doctor will decide when you can restart work and physical activities.
Contact your doctor if you experience the following:
- Fever
- Swelling, bruising or pain at the puncture site
- Shortness of breath or chest pain.
To avoid exacerbation of coronary artery disease and the onset of new coronary narrowings, cardiovascular risk factors should be controlled as best you can. You need to stop smoking, to ensure your bad cholesterol is very low, to balance diabetes and high blood pressure, to avoid becoming overweight and to resume physical activity. Follow-up with a cardiologist is essential.
Angioplasty can be completed in outpatients or during a short, 24-hour admission. Depending on the complexity of the lesions or the treatment you are taking, it can be performed immediately after coronary angiography or can be delayed.
The principle of the examination is the same as in coronary angiography: an introducer placed in the radial or femoral artery makes it possible to insert long flexible catheters into the coronary arteries. Injecting iodine and using X-rays makes it possible to locate the narrowings and position the angioplasty balloons and/
At the end of the procedure, the introducer is removed and compression of the artery is necessary to prevent the formation of a haematoma. Monitoring is required for a few hours after angioplasty. After the procedure, your cardiologist will prescribe dual antiplatelet treatment for a set period of time.
Performed in the operating room under general anesthesia, bypass surgery or surgeries is/are performed using the right and left internal mammary artery/arteries, in some cases, the right gastroepiploic artery, or a vein taken from the leg.
Surgery must be performed on a stopped heart, with extra-corporeal circulation (ECC) which temporarily ensures the role of the heart and lungs. In some cases, this procedure can also be performed with a beating heart if the patient’s technical circumstances so require.
Some coronary lesions need to be treated with coronary bypass surgery. For example, narrowings of the left coronary trunk and/or several other major arteries are generally worth operating on, especially in patients with diabetes or recurrences after angioplasty (stents).
What does coronary bypass surgery involve?
Coronary bypass surgery is a surgical procedure that consists of improving myocardial perfusion with new arterial grafts (ducts). Implanted away from areas of narrowing, these grafts bypass the obstruction in the coronary arteries. Depending on the number of coronary arteries affected, one to five bypasses can be performed at the same time.
What ducts are used?
In most cases, bypass grafts use:
- the internal thoracic artery: there are two of these, the left and right internal thoracic arteries; they are taken from the anterior chest wall. This is the most commonly used source for the graft, given its longevity
- the saphenous vein, taken from the leg
- the gastroepiploic artery, taken from the stomach
- the radial artery, taken from the forearm.
What happens during the operation?
It is performed under general anaesthesia and requires an incision in the middle of the sternum (sternotomy). Other incisions may be needed, depending on the graft used. In most cases, the heart is stopped to perform fine sutures (anastomoses) and extracorporeal circulation is installed to work on the heart and lungs during the procedure.
In some specific cases, the operation can also be performed without extracorporeal circulation; this is known as a “beating heart bypass”. Even so, it still requires a sternotomy.
The surgery takes three to six hours, depending on the complexity of the case.
Your stay in intensive care
After surgery, patients are admitted to an intensive care unit for about 48 hours. Assisted ventilation on a respirator continues for the first few hours and you will be weaned off gradually, by removing the tube from your mouth.
Medications are prescribed to relieve the pain, depending on symptoms and the VAS (pain rating scale). Intravenous fluids are also administered to maintain hydration.
Temporary drainage tubes (chest drains) are left in place for a few days, to remove the serous fluids and blood released from the surgical site after the operation. A small percentage of patients may require a blood transfusion. Oral nutrition can usually restart the day after the operation.
Returning to your room
After 48 hours, most patients will be allowed to get up and walk around, as long as the doctor agrees.
Regular physiotherapy sessions are helpful to recover functional autonomy and respiratory function. However, patients’ mobility remains limited by the electrodes for continued monitoring of their ECG (telemetry) and the drips needed for treatment. The same goes for the pain and insomnia, which reduce over time.
Is coronary bypass surgery risky?
Like all other surgical procedures, coronary revascularisation by implantation of the thoracic arteries or venous bypasses entails a risk of morbidity or mortality, the possibility of which are evaluated by the medical team (surgeon, anaesthetist and cardiologist) according to the condition of the patient’s heart and their overall health.
These complications can occur during or soon after the procedure.
Some of them, such as heart rhythm disorders (arrhythmia, bradycardia) may require the placement of a pacemaker; other, rarer ones may also occur, such as post-operative infections or neurological complications.
These risks, which the patient and their caregivers will be told about, are much lower than the risk of spontaneous progression of the disease that resulted in the recommendation of surgery.
What happens when you leave the Centre?
Patients are either discharged home or to a specialist convalescence centre, depending on their health or wishes.
Physical recovery is usually quick. Patients can start driving again from week 4, along with sexual activity. The main limitation to the resumption of normal activity is the healing of the sternum.
Like any bone fracture, it can take between 6 and 12 weeks to consolidate permanently. As such, any activity that places the ribcage under major strain is not allowed at the time.
Returning to work
This depends on how quickly an individual recovers and on how physical and stressful your job is. Sedentary activity can resume after four to six weeks. However, a job requiring strenuous physical activity will require around 12 weeks of rest. A consultation with your cardiologist will help set the date you can return to work.
Will I need rehabilitation?
A cardiac rehabilitation programme can help to track progress and to return to a normally active life sooner. You will also receive advice and recommendations on a new lifestyle: diet, weight loss and level of physical exercise or sport to be achieved. Your cardiologist and surgeon will advise you on adopting this rehabilitation programme, depending on the condition of your heart and your overall health.
Does coronary bypass surgery permanently cure coronary artery disease?
No. Coronary bypass surgery improves blood perfusion from the heart muscle, relieves symptoms and in some cases improves life expectancy. Almost all patients will need to take aspirin daily and for life (75 to 100 mg). Other medications may also be prescribed (drugs to lower your cholesterol or beta-blockers).
Long-term follow-up
All patients should be seen by their GP at regular intervals to check the risk factors, and by their cardiologist to assess the condition of their heart.
After coronary bypass surgery, most patients lead a normal, healthy and symptom-free life and can return to full professional activity.
Over time, atherosclerosis can continue to develop in the coronary arteries and grafts. After coronary angioplasty or coronary bypass surgery, it is therefore essential to limit the risk factors that can result in the exacerbation of atherosclerosis. These measures involve:
- losing weight (if overweight)
- stopping smoking
- lowering your cholesterol
- maintaining normal blood pressure
- dealing with diabetes, if you have it
- taking gentle, regular physical activity
- a balanced diet.