The Monaco Cardiothoracic Centre treats patients who are suffering from vascular diseases. Cardiovascular disease affects the heart and blood vessels. It is the leading cause of death in the world.
What are the different types of cardiovascular disease?
What are the risk factors?
What are the common symptoms?
How is it diagnosed?
What treatment is available?

WHAT IS VASCULAR DISEASE?
Cardiovascular disease is a group of disorders affecting the heart and blood vessels. Generally speaking, it includes sclerosis (pathological hardening of a tissue, organ), stenosis (narrowing of a duct or orifice), occlusion of arteries or veins, or their dilatation (aneurysms).
Which include, for example :
- Aortic dissection (partial tear of the aorta wall)
- Abdominal aortic aneurysm
- Deep vein thrombosis (or phlebitis)
- Pulmonary embolism
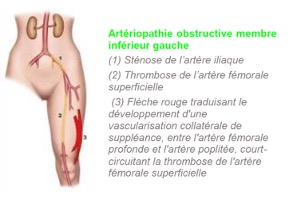
- Arteritis of the lower limbs, carotid arteries
- Ischemia (cessation or insufficiency of blood circulation to an organ)
- Heart failure
- Heart rhythm disorders
What is arteritis?
Causes
There are several risk factors : age, smoking, high blood pressure, high cholesterol, diabetes, physical inactivity and excess weight.
Early detection, even if asymptomatic, by a doctor and angiologist (vascular doctor) is important in case of cardiovascular risk factors.
Early symptoms
At the beginning of the disease, arteritis of the lower limbs causes no symptoms. Their onset is gradual when the narrowing of the affected artery hinders the flow of blood. When symptoms appear, they start to become more and more severe.
The disease first manifests as pain in certain leg muscles (the calves), a little like muscle cramps. This often occurs when walking uphill (sometimes when climbing stairs) and gradually increases, forcing the person to stop.
It resolves within ten minutes (usually in one to three minutes) at rest, then recurs when resuming exercise; this is referred to as ‘intermittent claudication’.
The pain always recurs when walking the same distance; we call this ‘walking perimeter’, which indicates the extent of the arteritis. These symptoms are exacerbated by the cold, altitude or wind, and in the postprandial period (after a meal). Gradually, the walking perimeter reduces (the more advanced the arteritis, the shorter the distance).
Symptoms then appear even at rest
When the disease progresses, muscle pain persists at rest. A pain resembling a burn often occurs in the foot, after a few minutes to a few hours laying down (usually at night). Sometimes, one foot is always colder than the other. It forces the person to get up several times a night, then to leave their leg hanging out of the bed. It is often resistant to painkillers and demonstrates exacerbation of the disease if it persists for more than 15 days.
Disorders related to poor vascularisation sometimes manifest in the feet, including:
- Changes to the skin, which becomes dry and pale; it peels and loses its hair (the regrowth of which is also slower)
- Tendency for the toenails to become brittle
- Decrease in skin temperature compared to the opposite foot not affected by arteritis
- Pale toes (or the entire foot) when the leg is raised, or conversely, they turn purplish-blue when the leg is tilted (hanging out of the bed or when standing up).
At a more severe stage, arteritis of the lower limbs can also cause:
- delayed healing of any minor wounds
- the onset of deep ulcers (areas where the skin loses its substance), usually in the foot.
There is then a major risk of amputation if treatment is not given quickly.
Diagnosis
A Doppler echocardiography is an examination that will diagnose arteritis. It consists in observing certain arteries and their blood flow on moving images.
In the case of arteritis of the lower limbs, stenosed or thrombosed arteries, are responsible for a drop in systolic pressure in the arteries of the foot and is lower than that found in the upper limbs, systolic pressure index is less than 0.9.
For an accurate diagnosis of arteritis of the lower limbs, an angioscanner is also necessary with an injection of a contrast medium.
When arteritis of the lower limbs is diagnosed, a general assessment of atherosclerotic cardiovascular disease must be carried out by looking at personal and family history, a biological assessment (cholesterol and triglyceride measurements, blood sugar measurement), search for cerebrovascular clinical signs (stroke: loss of vision, small aphasia or paralysis in the hand) or coronary disease (myocardial infarction, chest pain) that may have gone unnoticed.
Follow-up and treatment
When it is symptomatic and disabling, particularly in the case of severe limitation of the ability to walk distances, despite several months of well-monitored medical treatment, or in case of signs of ischemia (pain at rest, skin lesions) revascularization surgery should be considered.
Three techniques are available :
- dilatation or angioplasty,
- bypass surgery
- endarterectomy
What does this mean?
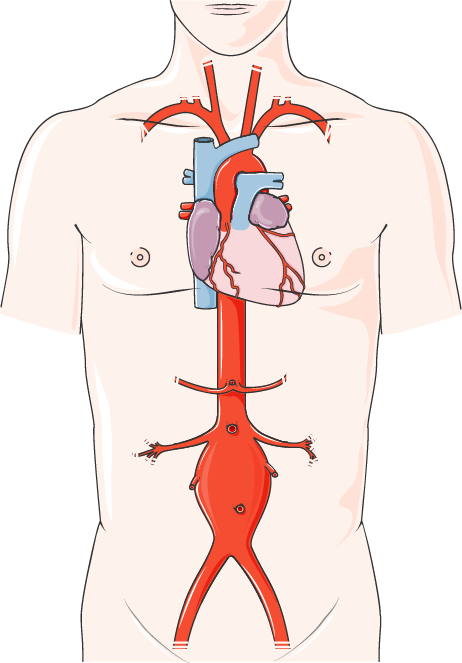
An abdominal aortic aneurysm is a dilation of the aorta, the main blood vessel that passes through the abdomen. It occurs when the wall of the aorta is damaged and weakened.
Causes
The exact causes of an abdominal aneurysm are unknown, even though this is important. Dilation may be due to weakness of the aortic wall, at a point where it is damaged. It can be caused by certain factors such as:
- High blood pressure
- Smoking
- High cholesterol
- Uncontrolled diabetes
- Obesity
- Stress
- Age
- A family history of vascular disease (genetic factors not yet identified).
Symptoms
An abdominal aortic aneurysm is almost always completely asymptomatic. Most people who have an abdominal aortic aneurysm have no symptoms. Aneurysms often develop slowly and go unnoticed. It is a silent disease until the day it ruptures. It is often detected during medical imaging examinations requested for another reason.
The only time it causes symptoms is when the aneurysm ruptures.
When an abdominal aneurysm increases in volume (and is therefore at risk of rupture), the patient can feel insidious pain and perceives a beating mass in their abdomen, in the middle or lower stomach, pain in the lower back or genitals or difficulty walking caused by pain in the legs during exertion.
- Intense pain in the lower back and abdomen
- Rapid pulse
- Loss of consciousness
- Weakness and severe sweating
- Pale skin
A sudden, sharp pain in the abdomen and back can mean that the aneurysm has ruptured or cracked. There is a serious risk of death, and the patient must undergo surgery as an extreme emergency to stop the haemorrhage.
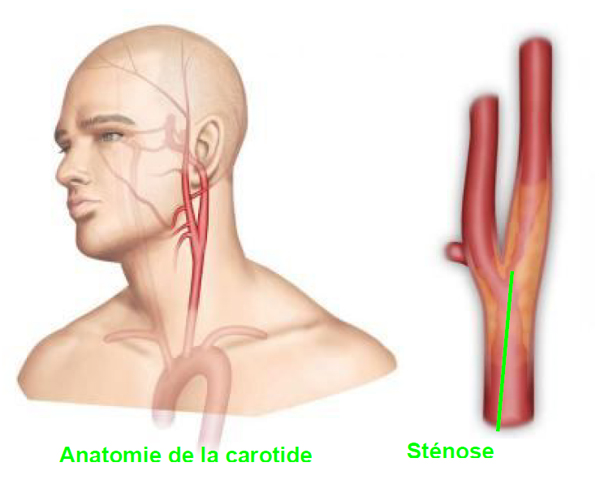
What is carotid stenosis?
The internal carotid artery is located in the neck. It goes up to the brain to provide the oxygen necessary for its proper functioning. It measures on average 4 mm in diameter. This artery can become clogged with fat deposits on the artery wall or by an atherosclerotic plaque, which leads to progressive narrowing of the artery (stenosis).
Causes
Carotid stenosis is linked to cardiovascular risk factors: smoking, high blood pressure, diabetes, high cholesterol, excess weight and a sedentary lifestyle. The frequency of strokes related to damage of the arteries supplying the brain appears more often after the age of 65.
Symptoms
- numbness in the face, arms or legs, especially on one side of the body;
- confusion, difficulty speaking or understanding speech;
- visual difficulties in one or both eyes;
- difficulty walking, dizziness, loss of balance or coordination;
Diagnosis
Doppler echocardiography is a simple and painless examination which measures the severity of stenosis by assessing the percentage of narrowing of the artery. This element is crucial as it will define the course of action to be taken.
If the stenosis is greater than 60%, an angioscan (or Magnetic resonance angiography) will be requested to determine its extent, to analyse the other arteries irrigating the brain as well as cerebral tissue in order to assess the consequences of the stenosis on the vascularization of the brain.
Follow-up and treatment
Treatment choice depends on two main criteria :
- evaluation of the percentage of stenosis,
- and whether or not it is symptomatic.
The indication for treatment also depends on the morphology of the atherosclerotic plaque as well as general criteria common to all surgical procedures (age, cardiac and respiratory status etc …).
The choice of treatment will be made with the vascular surgeon during an informed discussion on the various therapeutic possibilities, by evaluating the benefits and risks of the proposed treatment.
There are three possible techniques :
- medical treatment via antiplatelet agents,
- surgical treatment,
- carotid angioplasty with stenting.
DIAGNOSIS
Doppler echocardiography is an imaging examination that both shows and documents the appearance of the vessels and calculates the speed and direction of blood flow.
What is carotid Doppler echocardiography?
Carotid Doppler echocardiography is an imaging examination performed for diagnostic purposes, to view the carotid arteries in the neck. The aim of this test is to identify narrowings or blockages caused by the accumulation of plaques of atherosclerosis (clumps of cholesterol and calcium) associated with coronary artery disease.
It occupies a prominent, leading position in the analysis of arteries, and in the diagnosis and monitoring of carotid artery disease.
This examination goes beyond simple ultrasound because the device measures blood flow via the Doppler effect. This physical phenomenon is based on the calculation of the change in frequency of ultrasound waves (high-frequency sound waves) reflected by a moving target, for example the walls of the heart. Doppler ultrasound therefore provides important extra information that cannot be gathered from images alone. The Doppler effect makes it possible to study blood circulation, by quantifying the flow rate and accurately measuring the diameter of the blood vessels.
What happens during Doppler echocardiography?
- Doppler ultrasound is a simple, painless examination that works like any other ultrasound, using a probe placed against the skin over the area to be investigated. It is non-invasive (no X-rays; no injection of contrast medium).
- No preparation is required.
- The doctor first coats the skin over the area to be investigated with a gel, which improves the quality of the image and means the probe can be moved more quickly.
- Duration: 30 minutes.
- There are no side effects.
What is an echocardiogram?
Ultrasound of the heart, or an echocardiogram, is a medical imaging technique based on ultrasound, used to observe all the structures of the heart, i.e. the valves (aortic, mitral, etc.) and the cavities (the atria and ventricles). It also provides insight into the tone of the heart muscle.
Cardiac ultrasound is prescribed for symptoms that could suggest heart disease (e.g. chest pain, feeling unwell, etc.). It is very useful in the diagnosis of:
• heart failure
• congenital heart defects
• heart valve disease
• pericardial effusion.
Cardiac ultrasound is also used to assess the extent of lesions after a heart attack or to determine the impact of high blood pressure on the heart.
What happens during a cardiac ultrasound?
An echocardiogram is performed by a cardiologist at their office or by the patient’s bedside if in hospital.
It is usually performed via the transthoracic route. The doctor uses a probe that s/he places on the skin after covering it with a conductive gel, then moves it over the entire chest. This shows the various structures of the heart on a screen connected to the probe.
The transoesophageal route is sometimes preferred to get closer to the heart and obtain better images. This examination requires sedation and local anaesthesia of the throat: using an endoscope (a thin, flexible tube), the probe is placed into the oesophagus via the mouth until it comes close to the heart. The transoesophageal route is also used in people who are overweight or who have lung disease, which can interfere with transthoracic image quality.
- An echocardiogram takes about 30 minutes.
- No preparation is required before an echocardiogram. Note that if it is performed transoesophageally, the patient must not have had anything to eat, drink or smoke beforehand and must wait about an hour after the exam before they swallow anything, to prevent any risk of choking caused by the local anaesthetic in the throat.
- Cardiac ultrasound is non-invasive and does not cause any pain (although the transoesophageal route is a little unpleasant).
An echocardiogram is one of the examinations used to explore the heart, but does not provide an assessment of heart disease on its own. It must be combined with other exams, such as an electrocardiogram and coronary angiography.
CT scans and angiographies are medical imaging tests that use low doses of X-rays to create 3D images of the target areas. An angiographies provides a specific view of all the arteries in the human body.
What is an angio CT scan?

To observe the patient’s arteries, an injection of an iodine-based contrast medium is needed, for a better view of the arteries in the CT scan image. This product can be seen using X-rays, as it makes the structures it passes through opaque.
An angio CT scan is useful to search for vascular lesions such as aneurysms (localised dilation of an artery wall, making it very fragile and likely to rupture), narrowings in width (stenosis, usually related to plaques of atherosclerosis, the severity of which can be accurately quantified) or thrombosis (a clot forming in an artery and blocking it).
What happens during the exam?
- The examination is painless, quick and very useful to diagnose many conditions. It is almost completely non-invasive and only requires the placement of a catheter to inject the contrast medium into a vein.
- As it requires the injection of an iodine-based contrast medium, it is essential to check that there are no medical contraindications, which are rare. Caution should also be taken in patients with diabetes, kidney disease or a history of allergies.
- On the day of the test, only patients with allergies need to fast. Patients must not eat, drink or smoke for three to four hours beforehand.
- It is not unusual for the patient to experience a sensation of warmth when the contrast medium is injected, although the examination is still painless and not dangerous in any way. The patient is then placed on a moving table, under the circular radiology device. The part of the body to be examined is then moved within the scanner, shaped like a large ring that is open at both ends and contains a ray transceiver. Inside the ring, the transceiver rotates around the patient. Located behind a window to protect them from the X-rays, the radiologist ensures that everything runs smoothly. If there is any issue, the patient – who remains in constant contact with the medical team via a microphone – can tell them. Likewise, the team will tell the patient to keep still and when to hold their breath for a few seconds, to obtain higher quality images.
Once the exam is over, the drip is taken out and a small dressing is applied. - An angio CT scan takes less than half an hour.
- Patients should drink one to two litres of water after the exam to help the body eliminate the contrast medium.
- An angio CT scan does not pose much risk. Minor risk is associated with the administration of the contrast medium. Itching, redness or a bruise can occur near the injection site.
